Putting the Patient Back Together — Social Medicine, Network Medicine, and the Limits of Reductionism
Jeremy A. Greene, M.D., Ph.D., and Joseph Loscalzo, M.D., Ph.D.
From the Departments of Medicine and the History of Medicine and the Center for Medical Humanities and Social Medicine, Johns Hopkins University School of Medicine, Baltimore (J.A.G.); and the Department of Medicine, Brigham and Women's Hospital and Harvard Medical School, Boston (J.L.).
The New England Journal of Medicine, 2017 Dec 21;377(25):2493-2499.
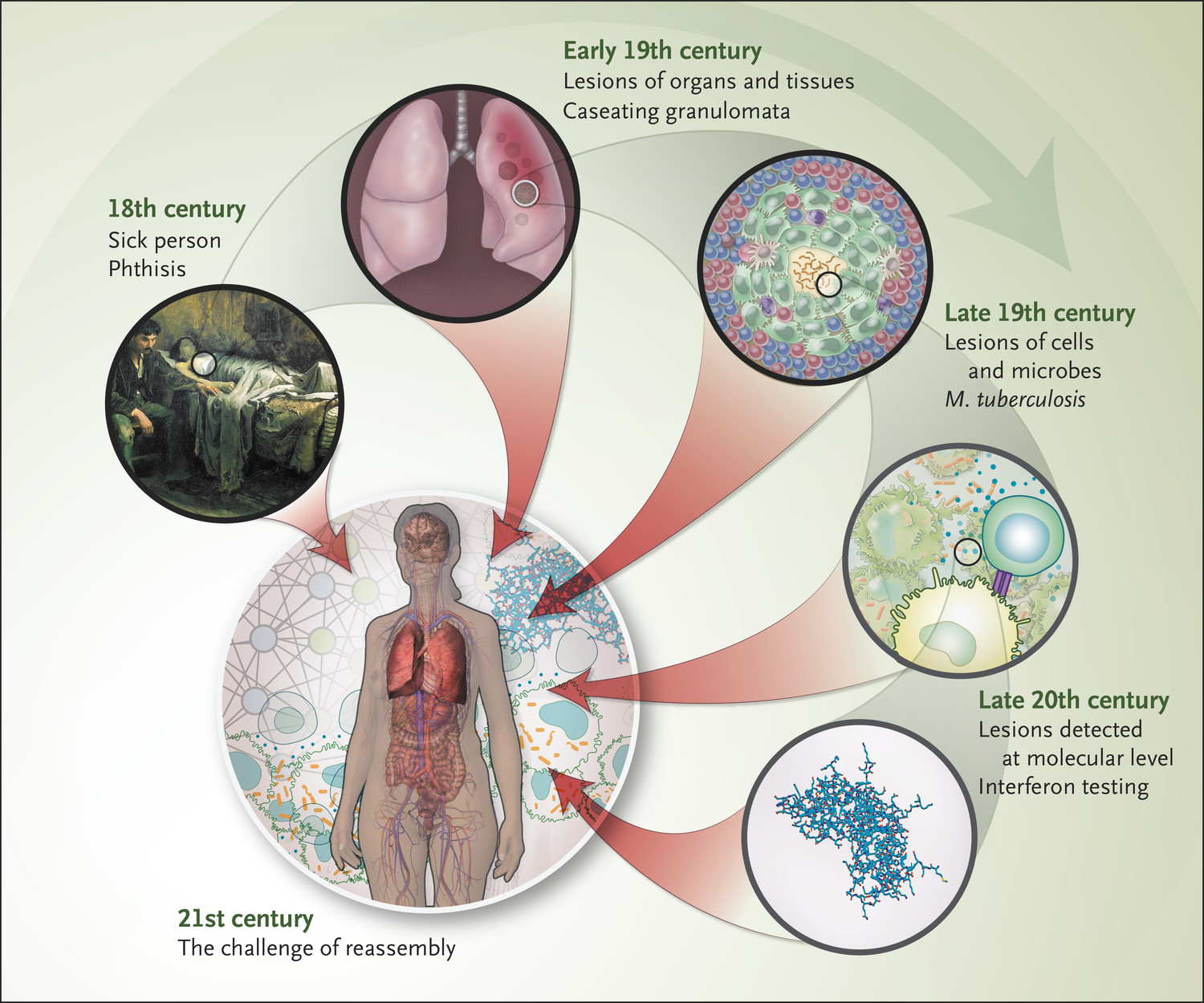
In the 21st century, the framework of biomedical research and clinical practice has begun to shift away from universal models of disease that generalize from close examination of diseased parts (organs, tissues, cells, or molecules) toward an approach that celebrates “personalized medicine” and focuses, at least nominally, on the whole person as a unit of analysis. Superficially, this transition appears to mark a return to the early modern conception of the patient as “sick person,” whose disease was considered inseparable from his or her complex constitutional inheritance and lived experience.
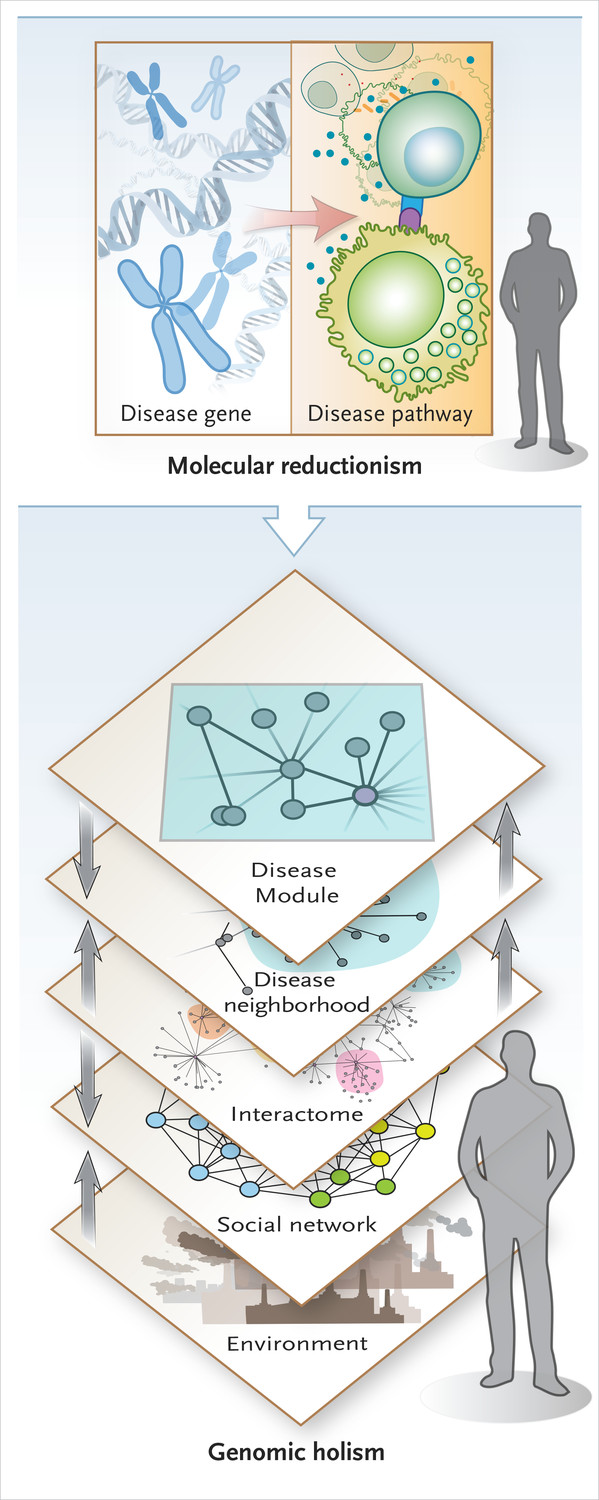
Yet in practice, personalized medicine still tends to reduce the patient to a collection of precise molecular sequences with detailed clinical phenotyping (“precision medicine”). As biomedical research and clinical practice try to assemble these atomized pieces into meaningful wholes, the process of putting the patient back together again has proven to be highly complex.
One disappointment of the postgenomic age is how little the Human Genome Project has taught us to date about human disease. Only a small minority of diseases are caused by monogenic (or oligogenic) disorders. Instead, complex interactions among numerous genetic and environmental factors determine disease phenotype. These observations, coupled with the increasing availability of bioinformatic data and high-throughput interaction screening, have led to calls for a new science of “network medicine” focused on the interrelational structures emerging from complex interactions among genes, proteins, internal milieu, and external environment.3 Network biologists echo a lineage of critical medical history, sociology, and anthropology that has long argued that biomedical reductionism misses crucial aspects of the etiology, pathobiology, prognosis, and treatment of human disease.
Critiques of reductionism by clinicians and social scientists and those from network biology, systems biology, bioinformatics, and complexity science seem to ignore each other almost completely. A potentially productive intersection between the two intellectual streams, however, has important implications for our post-omic future.